ICD 10 code for Abdominal Pain
The ICD 10 code for abdominal pain is a set of signs and symptom codes which can be coded only in the absence of a specific or definitive diagnosis.
Coding “Abdominal pain ICD 10”, does it confuse you?
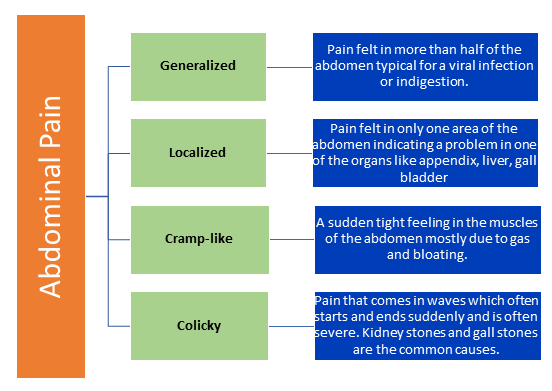
Abdominal pain is a common symptom that can be caused by a wide range of conditions. General causes of abdominal pain include gastrointestinal issues such as indigestion, gas, bloating, or constipation, as well as infections like gastroenteritis or urinary tract infections. In more severe cases, abdominal pain can be indicative of serious medical conditions such as appendicitis, pancreatitis, or gallstones.
Symptoms of abdominal pain can vary depending on the underlying cause but commonly include cramping, sharp or dull pain, bloating, nausea, vomiting, diarrhea, or constipation. The location of the pain in the abdomen can also provide clues to the potential underlying condition.
Potential underlying conditions associated with abdominal pain encompass a wide spectrum of organ systems and include:
- Gastrointestinal causes: Such as gastritis, peptic ulcers, inflammatory bowel disease, or irritable bowel syndrome.
- Gallbladder and liver conditions: Gallstones, cholecystitis, or hepatitis.
- Pancreatic disorders: Pancreatitis or pancreatic cancer.
- Appendicitis: Inflammation of the appendix, which often requires prompt surgical intervention.
- Urinary tract issues: Kidney stones, urinary tract infections, or bladder infections.
- Reproductive system problems: Ectopic pregnancy, ovarian cysts, or pelvic inflammatory disease.
- Vascular causes: Aortic aneurysm or ischemic bowel disease.
- Musculoskeletal causes: Strained muscles or hernias.
It is crucial to seek medical attention if abdominal pain is severe, persistent, or accompanied by other worrisome symptoms such as fever, blood in the stool, difficulty breathing, or persistent vomiting. Diagnostic tests such as physical examination, blood tests, imaging studies (e.g., ultrasound, CT scan), or endoscopic procedures may be required to determine the underlying cause of abdominal pain and guide appropriate treatment.
Does coding Abdominal pain ICD 10 confuse you? Understanding the documentation requirements and the code categories available in the ICD-10-CM manual will simplify the process.
Simply documenting “Abdominal pain” does not suffice the requirements for accurate coding. The location and the type also need to be specifically documented and to make things easier, it is also important that the terminologies used to document the location and type matches the descriptions in the ICD-10-CM manual.
For example if a physician orders a CT scan of the abdomen, the order should specifically mention if the CT scan is done for a generalized abdominal pain or pain in the right upper quadrant, right lower quadrant, left upper quadrant, left lower quadrant, epigastric or periumbilical regions. At the same time, the diagnosis supporting medical necessity should also specify the location and the type of the abdominal pain which is consistent with the order.
Always remember our goal is to avoid the unspecified codes and code the most specific code for the condition which will meet the medical necessity for any tests/procedures performed and the management of the condition.
ICD-10 Coding for Abdominal Pain
When coding for abdominal pain, it is important to first identify the location, severity, duration, and associated symptoms to determine the most appropriate code. The ICD-10 codes for abdominal pain are classified under different categories based on the underlying cause or source of the pain. The main categories include codes for generalized abdominal pain, right upper quadrant pain, left upper quadrant pain, right lower quadrant pain, left lower quadrant pain, periumbilical pain, epigastric pain, other specified abdominal pain, and unspecified abdominal pain. Let’s delve deeper into each category:
- Generalized abdominal pain:
Codes R10.0 and R10.00–R10.04 are used to classify generalized abdominal pain without further specification of the location or cause. These codes are used when the exact source of the pain is unknown or when the patient presents with diffuse abdominal discomfort.
Example: A patient presents to the emergency department with complaints of generalized abdominal pain. The physician documents the symptoms as diffuse and nonspecific. In this case, the appropriate ICD-10 code to use would be R10.0 – Acute abdomen.
- Right upper quadrant pain:
Codes R10.10–R10.13 are used to describe abdominal pain in the right upper quadrant, which may be indicative of conditions affecting the liver, gallbladder, or duodenum.
Example: A patient with a history of gallstones presents with severe right upper quadrant pain. The provider orders imaging studies that confirm acute cholecystitis. The correct ICD-10 code to use in this case would be R10.11 – Right upper quadrant pain.
- Left upper quadrant pain:
Codes R10.20–R10.23 are used to indicate abdominal pain in the left upper quadrant, which may be associated with conditions affecting the spleen, stomach, or pancreas.
Example: A patient with a history of pancreatitis presents to the clinic complaining of persistent left upper quadrant pain. After evaluation, the provider diagnoses chronic pancreatitis. The appropriate ICD-10 code to use would be R10.22 – Left upper quadrant pain.
- Right lower quadrant pain:
Codes R10.30–R10.33 are used for coding abdominal pain in the right lower quadrant, which is often a sign of appendicitis or other conditions affecting the intestines or reproductive organs on the right side.
Example: A patient presents with classic symptoms of appendicitis, including right lower quadrant pain, nausea, and fever. The provider determines that surgery is necessary and documents the diagnosis of acute appendicitis. The correct ICD-10 code to use would be R10.32 – Right lower quadrant pain.
- Left lower quadrant pain:
Codes R10.40–R10.43 are used to denote abdominal pain in the left lower quadrant, which may be associated with conditions affecting the colon, ovaries, or bladder on the left side.
Example: A female patient presents with left lower quadrant pain and urinary symptoms. A pelvic exam reveals tenderness, and imaging studies confirm the presence of a left ovarian cyst. The appropriate ICD-10 code to use would be R10.42 – Left lower quadrant pain.
- Periumbilical pain:
Codes R10.8 and R10.81–R10.84 are used for coding periumbilical pain, which is pain located around the umbilical region. This type of pain can be a sign of various gastrointestinal or vascular disorders.
Example: A patient with a history of Crohn’s disease presents with severe periumbilical pain and bloody diarrhea. Further workup confirms an acute flare of Crohn’s disease. The correct ICD-10 code to use would be R10.82 – Periumbilical pain.
- Epigastric pain:
Codes R10.1 and R10.11–R10.14 are used to describe epigastric pain, which is pain located in the upper central abdomen below the ribs. This type of pain is often associated with gastrointestinal disorders such as gastritis or peptic ulcers.
Example: A patient with a history of gastritis presents with recurrent epigastric pain and bloating. Laboratory tests reveal elevated inflammatory markers, supporting the diagnosis of gastritis. The appropriate ICD-10 code to use would be R10.13 – Epigastric pain.
- Other specified abdominal pain:
Codes R10.8 and R10.89 are used for coding abdominal pain that does not fit into the above categories or requires further specificity in documentation.
Example: A patient with a history of inflammatory bowel disease presents with atypical abdominal pain located in the left hypochondriac region. After thorough evaluation, the provider determines the pain is due to an inflamed splenic flexure of the colon. The correct ICD-10 code to use would be R10.84 – Other abdominal pain.
- Unspecified abdominal pain:
Code R10.9 is used when the documentation does not provide enough detail to assign a more specific code. This code is used as a placeholder when the exact nature of the abdominal pain is unclear.
Example: A patient presents to the primary care clinic with complaints of mild abdominal discomfort without clear localization. The provider performs a thorough physical exam but cannot determine the source of the pain. In this case, the appropriate ICD-10 code to use would be R10.9 – Unspecified abdominal pain.
Regions and Quadrants (Abdomen and Pelvis)

Abdominal pain can be caused by anyone of the following conditions-
| Acute | Chronic | Progressive |
|---|---|---|
| · Abdominal aortic aneurysm | · Angina | · Cancer |
| · Appendicitis | · Celiac disease | · Crohn’s disease |
| · Cholangitis | · Endometriosis | · Splenomegaly |
| · Cholecystitis | · Gallstones | · Gallbladder cancer |
| · Cystitis | · Gastritis | · Hepatitis |
| · Diabetic ketoacidosis | · GERD | · Kidney cancer |
| · Diverticulitis | · Hiatal hernia | · Liver cancer |
| · Duodenitis | · Inguinal hernia | · Pancreatic cancer |
| · Ectopic pregnancy | · Irritable bowel syndrome | · Stomach cancer |
| · Fecal impaction | · Functional dyspepsia | |
| · Heart attack | · Ovarian cysts | |
| · Injury | · Pelvic inflammatory disease | |
| · Intestinal obstruction | · Peptic ulcer | |
| · Intussusception | · Sickle cell anemia | |
| · Kidney infection | · Ulcerative colitis | |
| · Kidney stones | ||
| · Liver abscess | ||
| · Mesenteric ischemia | ||
| · Mesenteric lymphadenitis | ||
| · Pancreatitis | ||
| · Pericarditis | ||
| · Peritonitis | ||
| · Pleurisy | ||
| · Pneumonia | ||
| · Pulmonary infarction | ||
| · Ruptured spleen | ||
| · Salpingitis | ||
| · Sclerosing mesenteritis | ||
| · Shingles | ||
| · Spleen infection | ||
| · Splenic abscess | ||
| · Colon injury | ||
| · Urinary tract infection | ||
| · Viral gastroenteritis |
ICD-10 Coding Guidelines for Abdominal Pain
When coding for abdominal pain in ICD-10, there are certain guidelines that need to be followed to ensure accurate code assignment. These guidelines are set forth by the Centers for Medicare and Medicaid Services (CMS) and the American Hospital Association (AHA), and following them is essential for proper coding:
- Code Selection: The primary goal of coding for abdominal pain is to identify the underlying cause of the pain. Codes should be selected based on the specific location, severity, duration, and etiology of the abdominal pain. It is important to assign codes that reflect the highest level of specificity based on the available documentation.
- Acute v/s Chronic: It is crucial to differentiate between acute and chronic abdominal pain when assigning codes in ICD-10. Acute abdominal pain is sudden in onset and severe, while chronic abdominal pain is persistent or recurrent over a longer period of time. Accurately documenting the timing and nature of the pain is essential for proper code assignment.
- Underlying Cause: In many cases, abdominal pain is a symptom of an underlying condition or disease. It is important to document the suspected or confirmed cause of the abdominal pain, such as gastritis, appendicitis, cholecystitis, or other gastrointestinal disorders. Assigning a code for the underlying cause is crucial for accurate coding.
- Signs and Symptoms: In addition to documenting the specific cause of abdominal pain, healthcare providers should also document any associated signs and symptoms, such as nausea, vomiting, fever, or changes in bowel habits. These additional details can help in assigning more specific diagnosis codes in ICD-10.
- Documentation Quality: Thorough and detailed documentation is essential for accurate coding of abdominal pain in ICD-10. Healthcare providers should document the location, severity, duration, and radiation of the pain, as well as any factors that worsen or alleviate the pain. Clear and specific documentation will help in selecting the most appropriate diagnosis codes.
Documentation Requirements for Abdominal Pain
In order to accurately code for abdominal pain in ICD-10, healthcare providers must ensure that their documentation meets specific requirements. Comprehensive documentation not only supports accurate code assignment but also facilitates communication among healthcare providers and ensures proper care for the patient. Here are some key documentation requirements for abdominal pain:
- History of Present Illness (HPI): The HPI should include a detailed description of the abdominal pain, including the onset, location, character, severity, duration, and any aggravating or alleviating factors. Healthcare providers should document any associated symptoms, such as nausea, vomiting, diarrhea, or changes in bowel habits.
- Past Medical History: Documenting the patient’s past medical history is important for understanding the potential causes of abdominal pain. Healthcare providers should document any relevant medical conditions, surgeries, or medications that may contribute to or exacerbate the abdominal pain.
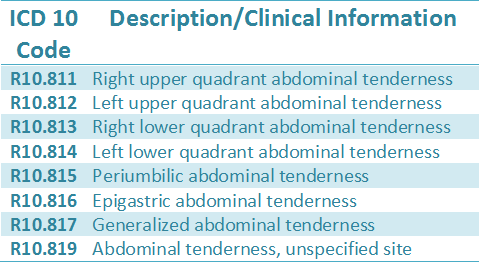
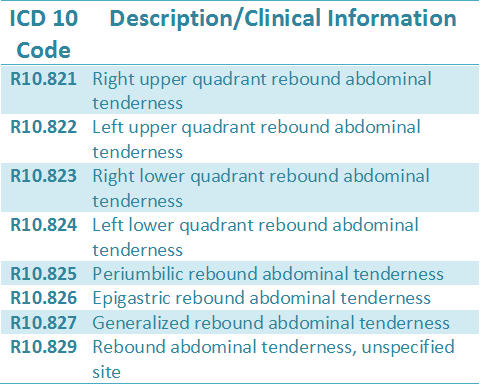
- Physical Examination Findings: The physical examination should include an assessment of the abdomen, including inspection, palpation, percussion, and auscultation. Healthcare providers should document any findings, such as tenderness, rigidity, rebound tenderness, or abnormal bowel sounds, that are relevant to the abdominal pain.
- Diagnostic Tests: If diagnostic tests are performed to evaluate the abdominal pain, the results should be documented in the patient’s medical record. This includes laboratory tests, imaging studies (such as CT scans or ultrasounds), and other diagnostic procedures that help in diagnosing the underlying cause of the pain.
- Treatment and Follow-up: Healthcare providers should document any treatments provided for the abdominal pain, including medications, procedures, or referrals to specialists. Additionally, follow-up instructions and plans should be clearly documented to ensure continuity of care and appropriate follow-up for the patient.
- Coding Documentation: In addition to clinical documentation, it is important for healthcare providers to document their thought process when assigning diagnosis codes for abdominal pain. This includes documenting the rationale for code selection, any uncertainties or considerations in code assignment, and any additional information that supports the chosen codes.
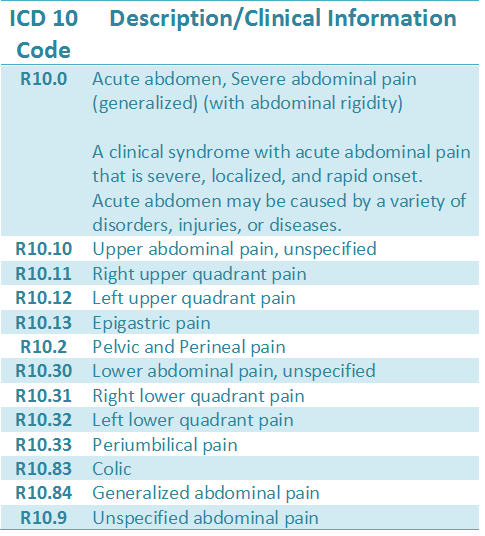
Organization of the abdominal pain codes in the ICD-10 manual
The abdominal pain codes belong to the category R10 (Abdominal and Pelvic pain)
The ICD 10 code for abdominal pain is arranged in the ICD-10 manual based on the severity of the pain. The list starts with the code R10.0 which represents the most severe or painful condition acute abdomen. The 4th digits 1,2 and 3 represents upper abdomen, pelvis and perineum and lower abdomen respectively and the digit 8 covers the other conditions- colic, generalized pain, tenderness, and rebound tenderness.
The definitions of the terms pertaining to abdominal pain and the related ICD 10 code for abdominal pain are below-
ICD 10 Code for Abdominal pain with descriptions:
Coding for Acute v/s Chronic Abdominal Pain:
Acute and chronic abdominal pain are two distinct medical conditions that require different approaches to diagnosis and treatment. In the realm of medical coding, the differentiation between acute and chronic abdominal pain is crucial for accurately capturing the patient’s condition and ensuring proper reimbursement. This article will delve into the nuances of ICD-10 coding for acute and chronic abdominal pain, including an analysis of the key differences between the two and common ICD-10 codes used for each category.
Distinguishing Between Acute and Chronic Abdominal Pain:
Acute abdominal pain is characterized by sudden onset and is usually severe in intensity. It is often associated with a specific cause such as trauma, infection, inflammation, or obstruction. On the other hand, chronic abdominal pain persists over a prolonged period, typically lasting for more than three to six months. Chronic abdominal pain may be intermittent or constant and is often more challenging to diagnose due to its long-standing nature.
ICD-10 Coding for Acute Abdominal Pain:
When coding for acute abdominal pain in ICD-10, it is important to identify the underlying cause or condition that is responsible for the pain. Specificity is key in coding acute abdominal pain to ensure accurate reimbursement and clinical documentation. Some common ICD-10 codes used for acute abdominal pain include:
K59.1 – Functional dyspepsia: This code is used to indicate acute abdominal pain that is related to functional gastrointestinal disorders such as dyspepsia or non-ulcer dyspepsia.
R10.0 – Acute abdomen: This code is a general code used to indicate acute abdominal pain without specifying the underlying cause. It is often used as a placeholder until a definitive diagnosis is made.
K58.0 – Irritable bowel syndrome with diarrhoea: This code is used to indicate acute abdominal pain associated with irritable bowel syndrome that presents with diarrhea as a predominant symptom.
R10.10 – Upper abdominal pain, unspecified: This code is used when the location of the pain is not clearly defined but is in the upper abdominal region.
R10.30 – Lower abdominal pain, unspecified: Similar to the code for upper abdominal pain, this code is used when the location of the pain is in the lower abdominal region.
ICD-10 Coding for Chronic Abdominal Pain:
Chronic abdominal pain poses a unique challenge in medical coding as it requires a comprehensive evaluation to identify the underlying cause and establish a treatment plan. When coding for chronic abdominal pain in ICD-10, it is essential to document the duration of the pain, any exacerbating or alleviating factors, and associated symptoms. Common ICD-10 codes used for chronic abdominal pain include:
R10.81 – Generalized abdominal pain: This code is used to indicate chronic abdominal pain that is diffuse and not localized to a specific area.
K58.9 – Irritable bowel syndrome without diarrhea: This code is used for chronic abdominal pain associated with irritable bowel syndrome where diarrhea is not a predominant symptom.
K59.00 – Constipation, unspecified: Chronic abdominal pain can be a presenting symptom of chronic constipation, and this code is used to indicate this condition.
K31.9 – Disease of stomach and duodenum, unspecified: Chronic abdominal pain originating from the stomach or duodenum may be indicated using this code when a specific diagnosis is not available.
K59.1 – Functional dyspepsia: This code can also be used for chronic abdominal pain related to functional gastrointestinal disorders, particularly dyspepsia.
Key Differences in ICD-10 Coding for Acute and Chronic Abdominal Pain:
- Duration: The primary difference between coding for acute and chronic abdominal pain lies in the duration of the pain. Acute pain is sudden in onset and typically resolves within a short period, whereas chronic pain persists for an extended period, often lasting for months or even years.
- Specificity: Coding for acute abdominal pain often requires more specificity to identify the underlying cause or condition responsible for the pain. In contrast, chronic abdominal pain may necessitate a broader approach to capture the long-standing nature of the pain and associated symptoms.
- Documentation: Physicians and coders must collaborate closely to ensure accurate documentation of the patient’s symptoms, medical history, and diagnostic findings when coding for chronic abdominal pain. Comprehensive documentation is crucial for accurately capturing the complexity of chronic pain conditions.
- Treatment Approach: The management of acute and chronic abdominal pain differs significantly, with acute pain often requiring urgent intervention to address the underlying cause, while chronic pain may necessitate a multimodal approach involving long-term pain management strategies.
Common Causes of Abdominal Pain: ICD-10 Codes for Gastritis, Appendicitis, and Gastroenteritis
Abdominal pain is a common symptom that can be attributed to a range of underlying conditions, both benign and serious. In this comprehensive guide, we will explore the common causes of abdominal pain, focusing on conditions such as gastritis, appendicitis, and gastroenteritis. We will delve into the clinical presentation, diagnosis, and management of these conditions, while providing relevant ICD-10 codes for each.
- Gastritis
Gastritis refers to inflammation of the stomach lining, which can be acute or chronic in nature. The most common symptoms of gastritis include abdominal pain, bloating, nausea, and vomiting. The diagnosis of gastritis is typically made based on clinical presentation, along with endoscopic findings and histology.
ICD-10 Code for Acute Gastritis: K29.00
ICD-10 Code for Chronic Gastritis: K29.70
Treatment of gastritis involves identifying and addressing the underlying cause, such as Helicobacter pylori infection, nonsteroidal anti-inflammatory drug (NSAID) use, or excessive alcohol consumption. Management strategies may include proton pump inhibitors (PPIs) to reduce gastric acid secretion, antibiotics for H. pylori eradication, and lifestyle modifications.
- Appendicitis
The classic presentation of appendicitis includes periumbilical pain that migrates to the right lower quadrant, accompanied by fever, anorexia, and localized tenderness on examination. Diagnosis is primarily based on clinical assessment, supplemented by imaging studies such as ultrasound or computed tomography (CT) scan.
ICD-10 Code for Acute Appendicitis: K35.80
Surgical intervention in the form of an appendectomy is the mainstay of treatment for appendicitis. In cases of complicated appendicitis with abscess formation or perforation, antibiotic therapy may be indicated. Early recognition and prompt surgical management are crucial to prevent complications such as perforation and peritonitis.
- Gastroenteritis
Gastroenteritis refers to inflammation of the stomach and intestines, usually caused by infectious agents such as bacteria, viruses, or parasites. Common symptoms of gastroenteritis include abdominal pain, diarrhea, vomiting, and fever. The diagnosis is often clinical, based on a thorough history and physical examination.
ICD-10 Code for Viral Gastroenteritis: A08.4
ICD-10 Code for Bacterial Gastroenteritis: A09
ICD-10 Code for Parasitic Gastroenteritis: A07
Management of gastroenteritis focuses on supportive care to maintain hydration and electrolyte balance. In cases of bacterial gastroenteritis, antimicrobial therapy may be considered based on the identified pathogen. Prevention strategies include hand hygiene, proper food handling, and vaccination for specific pathogens such as rotavirus.
ICD 10 code for abdominal pain – Examples:
- A 52-year-old female presents to the clinic with severe epigastric abdominal pain associated with nausea and vomiting. She rates the pain as 7-8/10 on the pain scale. She describes the pain as constant. The patient reports eating fried Turkey at her friend’s birthday party, 3 days ago.
The examination revealed abdominal distention and tenderness across the mid-upper abdomen with rigidity and diminished bowel sounds.
The patient was diagnosed with severe epigastric abdominal pain suspected of acute pancreatitis, epigastric abdominal tenderness and dehydration.
ICD-10-CM codes-
R10.13 – Epigastric abdominal pain ICD 10
R10.816 – Epigastric abdominal tenderness ICD 10
E86.0 – Dehydration ICD 10
Note: Acute pancreatitis is not coded as the condition is “suspected” and not confirmed.
- An 18-year-old male comes to the clinic with severe nausea and vomiting and pain in the right lower quadrant of his flank. He states that the pain began suddenly near the navel region and shifted to the lower right flank. He reports worsening of the pain when he coughs or walks. A CT scan of the flank was ordered. The ICD-10-CM codes on the order would be-
R10.31- Right lower quadrant abdominal pain ICD 10
Note: Flank pain is the same as abdominal pain as directed by the ICD-10-CM Index. So as per the guidelines, in the above example Flank pain ICD 10 coded with abdominal pain ICD 10 code.